Making Healthcare Simpler through Innovation
For the more than 40 million consumers in Anthem affiliated health plans, the way they shop for groceries, watch television or listen to music has changed dramatically during the past few years. Today, almost 80 percent of Americans own a smartphone and spend up to five hours per day "virtually" on their mobile devices. In a world that has become much more on demand and rapid delivery, Anthem's challenge is to create a healthcare experience that provides the same convenience and simplicity.
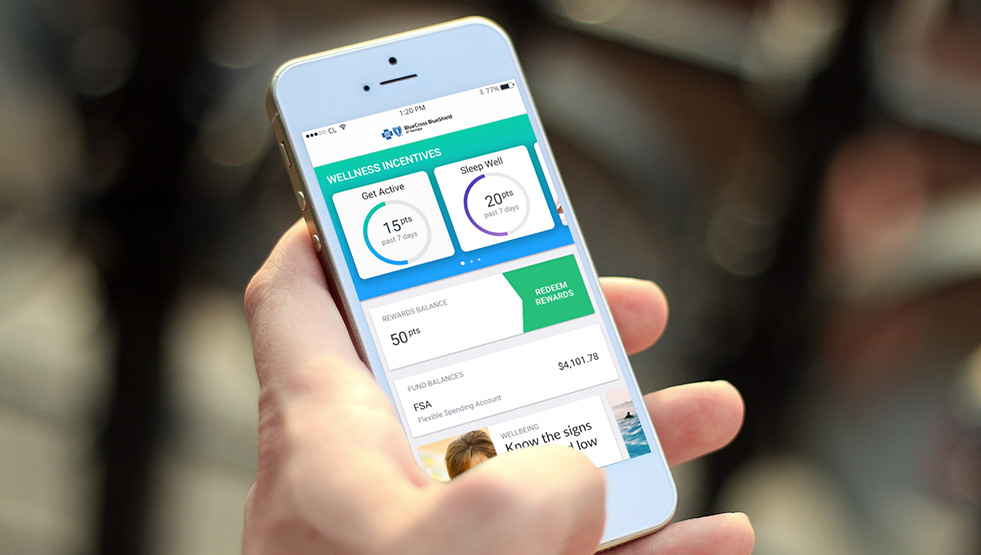
With this in mind, in 2017, Anthem launched Engage—a robust digital platform that combines information about a consumer's health plan, care provider network and personalized tools for health and well-being in one application.
"Consumers are busy, on-the-go people, and we want to streamline their health management so it fits seamlessly into their lifestyle," explains Tim Skeen, Anthem Senior Vice President and Chief Information Officer. "What's revolutionary about Engage is that it is the only app that covers in one place the full spectrum of an individual's health—from personal tools to manage wellness, to cost and quality information, and resources to manage specific health conditions. Engage essentially works as a personalized digital healthcare assistant."
Engage operates from a simple principle—individuals should be empowered to make decisions about their health and their healthcare that are right for them. Engage provides consumers with cost and quality information on care providers, in addition to details about their specific healthcare coverage, medical claims status, prescriptions, Health Savings Account balances, and employer benefits. Consumers can also access a wide range of Anthem programs and resources through the app, and can synchronize the app with fitness and health monitors to conveniently track exercise, food and sleep data to gain better insight into their overall health.
More than 800,000 Anthem consumers are already using Engage, and we expect that number to double in 2018.
 Shane Hornbuckle, an Atlanta-based Anthem consumer and father of three, credits Engage with saving him time and keeping his family's healthcare information organized.
Shane Hornbuckle, an Atlanta-based Anthem consumer and father of three, credits Engage with saving him time and keeping his family's healthcare information organized.
"Looking for healthcare after hours or checking on the status of health claims used to require a call to customer service or trying to remember how to access my account online," says Shane. "With the Engage app, I can easily find a care provider and access my coverage information. There's a sense of security that comes with knowing where everything is and having it at my fingertips anytime I need it."
Anthem recently introduced several other digital innovations with the same goal in mind—making the healthcare experience simpler. They include Pay My Bills, mobile bill-pay capabilities that allow consumers to pay premiums directly from their mobile device quickly and conveniently; What's My Status, which provides consumers with real-time updates on their claims; and No More Cards, which eliminates the need for a physical ID card by providing a digital card accessible through a consumer's mobile device. Consumers appreciate the convenience of these digital innovations, with nearly 195,000 premium payments processed to-date through Pay My Bills.
"The digital innovations that we launched in 2017 have been really well received by consumers," said Tim. "As the digital world around us continues to evolve and become more complex, we need to work even harder to deliver even more innovative solutions that exceed consumers' needs and lead our industry."
While digital innovation can be complex, the benefit for consumers is fairly simple. As Shane says, "receiving a text message notifying me that my claim is taken care of while at my child's track meet, allows me to cross that off my list of concerns and focus on what matters most. Anticipating and understanding my needs really sends an underlying message that Anthem cares."

