Health equity means everyone has a fair and just opportunity to be as healthy as possible.1 To deliver on this commitment, we need a healthcare system that is personalized to individuals, accounting for their attributes, experiences, characteristics, and preferences. Anchored by our mission to improve lives and communities and to expect more from ourselves, Anthem is accelerating this transformation by identifying and understanding how health inequities impact the people we serve.
Helping people remain independent and maintain quality of life is foundational to improving health. Addressing these needs through our Essential Extras benefits program, Anthem Medicare Advantage members in select plans can customize their approach to whole health by choosing from up to nine unique benefits. The Personal Home Helper benefit provides up to 31 visits of up to 4 hours each day of personal care services for those people who need help with two or more activities of daily living. The Healthy Pantry benefit provides nutritional counseling and a monthly delivery of nonperishable food staples to help those with chronic conditions make changes to their diet. Taken together, Essential Extras services provide support that help members live longer, healthier lives.
Housing instability can be one of the more pervasive obstacles to health. Last year, Anthem’s What’s Driving Our Health study found that nearly one in four people in the United States worried about losing their housing, while 41% said affordable housing is not always easily accessible to them.2
The Anthem Housing Flex Fund program addresses housing concerns for those who are experiencing — or at risk of — homelessness. Supported by local teams in 10 states, the program provides funds to assist with rent, utilities, moving expenses, and other housing-related costs.3 Anthem Community Engagement Navigators help members by connecting them to community resources and finding creative ways to address the underlying factors that negatively affect whole health and drive inequities.
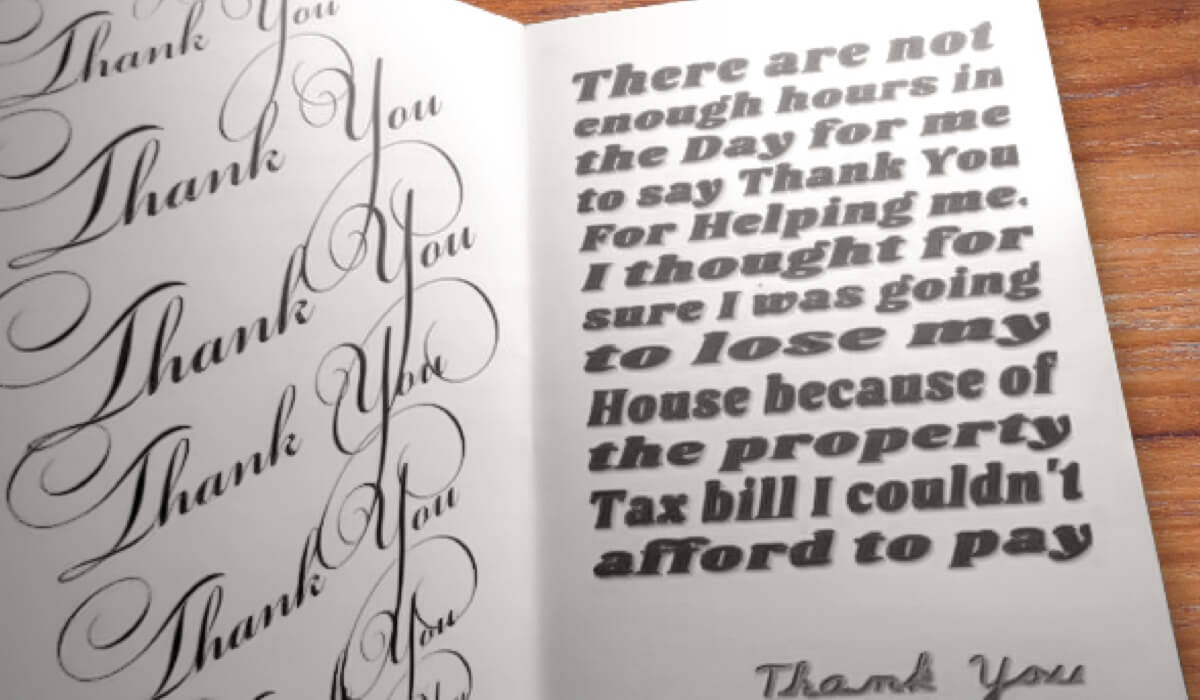
A member sent a homemade card expressing her gratitude for everyone involved in helping her keep her home.
Rebecca Boyd, an Anthem Community Engagement Navigator in Kentucky, works with individuals enrolled in our Medicaid and Medicare plans to understand barriers to their health, as well as any health-related social needs they may be experiencing. Over the course of several months, she helped a 61-year-old member obtain food and pay her utility bills and contacted a community group that installed safety assistive equipment in the member’s bathroom for free. When the member was about to lose her home because of an overdue tax bill, she turned to us.
With Rebecca’s help, the member gathered and submitted the documents needed so the tax bill could be paid with assistance from the Anthem Blue Cross and Blue Shield of Kentucky Housing Flex Fund.
“I’ve been a social worker for 20 years, and I’m still brought to tears when I hear about the challenges our members are going through,” Rebecca says. “I’m incredibly proud of the resources we offer to truly help support our members.”
“The healthcare system acting alone cannot eliminate all factors that drive disproportionately poorer outcomes for some people,” says Anthem Chief Health Officer Shantanu Agrawal, M.D. “Anthem is working every day to address social drivers of health, such as housing instability. We act with urgency to understand the unique experiences of our members, to foster and sustain a trusting relationship, and to effectively partner with them to optimize their health.”